Thirteen Facts Prostate Health
Thirteen important facts about male prostate health, a blog by CSB Aleena Aspley of North Brisbane Queensland Australia. Aleena is a Certified Somatic Sexologist / Sexological Bodyworker.
.
Thirteen Facts Prostate Health
1. PROSTATE FLUID KEEPS SPERM HEALTHY
Situated beneath the bladder, the prostate is a gland of approximate walnut size exclusive to males. Passing through it is the urethra, the conduit responsible for transporting urine from the bladder to the penis. Primarily, its function revolves around generating prostatic fluid, a vital substance that furnishes sperm with essential nutrients.
.
What a Healthy Sperm Looks Like
Thirteen Facts Prostate Health
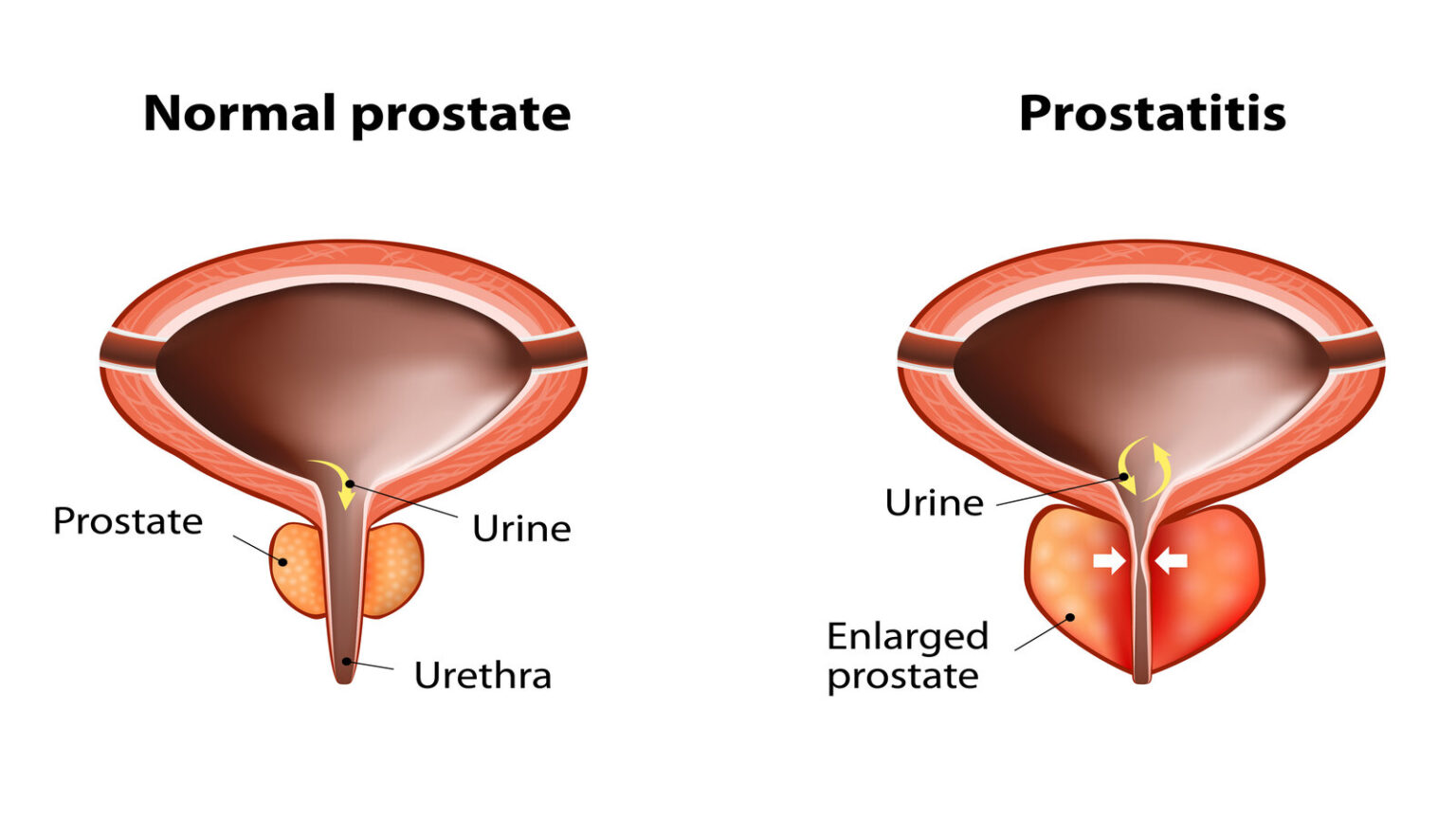
2. URINARY INFECTIONS & PROSTATE HEALTH
Prostatitis, characterized by the inflammation or infection of the prostate, predominantly impacts men below the age of 40 and can stem from urinary tract infections. Manifestations may encompass discomfort during urination and ejaculation, coupled with pelvic pain. The underlying triggers range from bacterial sources to sexually transmitted infections like gonorrhoea or chlamydia. Fortunately, antibiotics can effectively address and treat this condition.
.
.
3. PROSTATITIS AND PROSTATE CANCER
Emerging evidence points to a potential link between prostatitis and an increased susceptibility to prostate cancer. The presence of prostatitis, marked by inflammation or infection of the prostate, might elevate the risk of developing prostate cancer in certain individuals. This connection is underscored by the potential influence of chronic inflammation on the cellular environment of the prostate.
Furthermore, the association between prostatitis and prostate cancer risk gains complexity when coupled with the deficiency of vitamin D. Vitamin D deficiency has been linked to various health issues, including impaired immune function and heightened inflammation. In the context of prostatitis, the combination of inflammation and insufficient vitamin D levels might provide a conducive environment for the initiation and progression of prostate cancer cells.
While more research is needed to elucidate the precise mechanisms and interplay between prostatitis, vitamin D, and prostate cancer, these findings underscore the importance of proactive prostate health management. Engaging in practices that mitigate inflammation, such as maintaining a healthy lifestyle, including a balanced diet and sufficient physical activity, along with appropriate sun exposure for vitamin D synthesis, may contribute to reducing the potential risk of prostate cancer in individuals who have experienced prostatitis.
.
.
4. CONDOMS & MAINTAING GENITAL HYGIENE
Maintaining proper genital hygiene and using condoms can play a crucial role in preventing urinary tract infections (UTIs) and prostatitis, two conditions that can significantly impact prostate health. By adopting these practices, individuals can take proactive steps to safeguard their well-being and minimize the risk of developing these discomforting and potentially serious issues.
Genital hygiene is essential for preventing the accumulation of harmful bacteria in the genital area, which can potentially lead to infections. Regular cleansing and maintaining a clean, dry environment can help reduce the likelihood of bacteria entering the urethra and causing infections. Proper hygiene practices can also contribute to overall genital health and comfort, supporting the prevention of urinary tract infections and prostatitis.
Condom usage is another crucial aspect of prostate health maintenance. Condoms act as a barrier that helps prevent the transmission of sexually transmitted infections (STIs) and other harmful microorganisms that can lead to urinary tract infections and prostatitis. Engaging in safe sexual practices by consistently using condoms can significantly reduce the risk of infection and support overall prostate health.
Additionally, emerging research highlights the potential role of vitamin D in enhancing the body’s ability to resist infections. Vitamin D is known to play a vital role in supporting the immune system’s function, helping the body fend off harmful pathogens. Individuals with adequate levels of vitamin D may experience improved immune responses, which could contribute to a heightened ability to fight off infections, including those that affect the prostate and urinary tract.
By ensuring proper genital hygiene, practicing safe sexual behavior, and maintaining adequate vitamin D levels, individuals can take proactive measures to promote prostate health and reduce the risk of urinary tract infections and prostatitis. These preventive strategies not only contribute to overall well-being but also support the body’s natural defense mechanisms against infections, further underscoring the importance of a comprehensive approach to prostate care.
.
:max_bytes(150000):strip_icc()/how-to-correctly-size-a-condom-49115-ADD-FINAL2-c8f78f0841534ff98c858ed67318b3b3.png)
How to choose the right condom size?
.
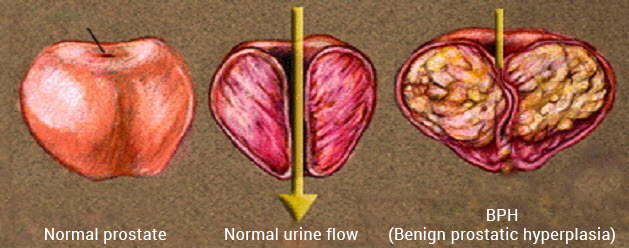
5. PROSTATE ENLARGEMENT & AGE
Benign prostatic hyperplasia (BPH), commonly referred to as an enlarged prostate, is a prevalent condition that affects a significant portion of men over the age of 60. It is estimated that at least 60 percent of men in this age group experience BPH, characterized by the enlargement of the prostate gland. As the prostate gland enlarges, it can exert pressure on the urethra, the tube responsible for transporting urine from the bladder to the penis, leading to a range of urinary symptoms.
Symptoms associated with BPH often include challenges with urination and an increased frequency of trips to the restroom. Men with BPH may find it difficult to initiate urination, experience a weak urinary stream, or have a sensation of incomplete emptying of the bladder. The frequent need to urinate, particularly during the night, can disrupt sleep patterns and negatively impact overall quality of life.
In cases where BPH symptoms are mild and not significantly affecting an individual’s well-being, active surveillance and lifestyle modifications may be recommended. Lifestyle changes such as reducing fluid intake before bedtime and avoiding caffeine and alcohol can help alleviate mild symptoms.
For men experiencing more severe BPH symptoms that substantially affect their daily routines and quality of life, medical intervention may be necessary. There are various treatment options available, including medications and surgical procedures. Medications aimed at reducing the size of the prostate gland or relaxing the muscles around the prostate can be prescribed to alleviate symptoms. Surgical interventions, such as transurethral resection of the prostate (TURP), may be recommended to remove excess prostate tissue and relieve urethral obstruction.
.
BPH — BENIGN PROSTATE HYPERPLASIA MASSAGE TO RELIEVE SWELLING
.
Individualized treatment plans are tailored to the severity of symptoms, the individual’s overall health, and their preferences. By effectively managing BPH, men can experience an improved quality of life and better urinary function, highlighting the importance of seeking medical advice and appropriate treatment for this common prostate condition.
.

Benign Prostatic Hyperplasia
.
6. THE MOST COMMON CANCER IN MEN
Prostate cancer is a significant health concern that affects a substantial portion of the male population. It is estimated that one in nine men will be diagnosed with prostate cancer at some point in their lives, making it a prevalent condition worldwide.
In Australia alone, approximately *20,000 new cases of prostate cancer are diagnosed annually. Tragically, the disease claims the lives of around 3,300 men each year, underscoring the importance of early detection and effective management. *(This blog was written in 2023)
Age plays a pivotal role in the prevalence of prostate cancer, with the majority of diagnoses occurring in older individuals. Almost two-thirds of those diagnosed are aged 65 and older, highlighting the increased susceptibility that comes with advancing age.
Certain demographic factors and genetic predispositions can contribute to an elevated risk of developing prostate cancer. Men of Afro-Caribbean descent, for instance, face an increased risk compared to other populations. Additionally, a family history of prostate cancer can amplify the likelihood of being diagnosed with the disease, as those with close relatives affected by prostate cancer are at a higher risk themselves.
Remarkably, early-life experiences can also influence one’s prostate cancer risk. Having a sexually transmitted infection (STI) during youth can serve as a risk factor for prostate cancer development later in life. This emphasizes the interconnectedness of various factors and underscores the need for proactive measures to protect prostate health.
The statistics surrounding prostate cancer serve as a stark reminder of the significance of regular health check-ups, screenings, and awareness campaigns. By being vigilant about risk factors, staying informed about family history, and maintaining a proactive approach to overall health, men can empower themselves to reduce their risk and contribute to early detection and successful treatment of prostate cancer.
.

Prostate Cancer Gene Expression Testing
.
7. GENETICS & PROSTATE HEALTH
The intricate relationship between genetics and prostate cancer is a topic of growing interest and research. It has been observed that a notable portion of prostate cancer cases, up to 10 percent, have a hereditary component. This suggests that certain genetic factors play a significant role in predisposing individuals to the development of this cancer.
One such example is the BRCA2 gene, which has garnered attention for its association with both breast cancer in women and prostate cancer in men. This gene, known to regulate the repair of damaged DNA, is crucial for maintaining the stability of the genome. Mutations in the BRCA2 gene have been linked to an increased risk of breast and ovarian cancers in women, as well as an elevated susceptibility to prostate cancer in men. This intriguing connection highlights the complex interplay of genetic factors that can influence the onset of various cancers.
The identification of these genetic links underscores the importance of understanding one’s family history and genetic predispositions when assessing the risk of prostate cancer. Individuals who have close relatives, particularly parents or siblings, with a history of prostate cancer should be particularly vigilant about regular health screenings and consultations with healthcare professionals. Genetic testing and counseling can provide valuable insights into an individual’s risk profile and guide personalized healthcare decisions.
As our understanding of the genetic underpinnings of prostate cancer continues to evolve, the medical community is better equipped to identify high-risk individuals, tailor treatment strategies, and develop targeted interventions that aim to mitigate the impact of hereditary factors on prostate health.
.
Prostate Cancer and the Importance of Early Detection
Thirteen Facts Prostate Health
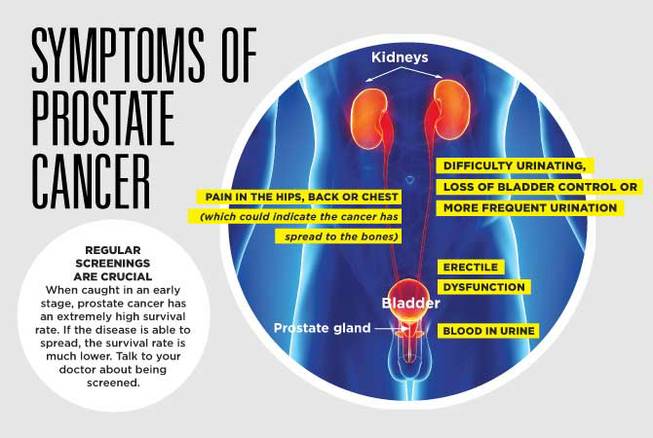
8. PROSTATE CANCER CAN ELUDE DETECTION AND BE SYMPTOMLESS
Prostate cancer, in its early stages, can often elude detection due to its subtle or even absent symptoms. While certain men may experience lower back or hip discomfort, the majority may remain asymptomatic during this crucial period of the disease. Recognizing the need for effective screening tools, medical professionals have turned to the PSA blood test as a valuable diagnostic tool.
The PSA blood test measures the levels of prostate-specific antigen, a compound produced by the prostate gland. Elevated PSA levels can serve as an indicator of potential issues within the prostate, including the presence of cancer. Regular PSA testing enables healthcare providers to monitor changes in PSA levels over time, helping to detect abnormalities and initiate timely interventions.
As prostate cancer advances, it can manifest in more noticeable ways. Individuals facing advanced prostate cancer may encounter a range of symptoms that demand attention. Bone, pelvic, or back pain may arise, often serving as a distressing signal of the disease’s progression. Weight loss, sometimes unexplained, can also occur, emphasizing the systemic impact of the condition.
Furthermore, the presence of blood in the urine or semen can be an alarming sign of advanced prostate cancer. These visible signs underscore the importance of seeking medical evaluation when such symptoms emerge. Early diagnosis and intervention remain pivotal in effectively managing prostate cancer and optimizing treatment outcomes.
While the subtlety of early symptoms poses a challenge, the combination of regular PSA testing, attentive symptom recognition, and proactive medical care offers individuals the best chance of detecting and addressing prostate cancer in its various stages. Timely medical attention empowers individuals to navigate the complex landscape of prostate health with greater awareness and confidence.
.

The PCA3 test for Prostate Cancer
.
9. THE PCA3 TEST IS A VALUABLE TOOL TO DETECT PROSTATE CANCER
In recent advancements in prostate cancer detection, a promising test known as PCA3 has emerged as a valuable tool for identifying the presence of cancer cells. This innovative test specifically targets a protein that is produced exclusively by cancer cells within the prostate gland. The accuracy of the PCA3 test has been reported to be approximately 80%, representing a significant improvement in diagnostic precision.
The PCA3 test offers a novel approach to prostate cancer detection by focusing on the unique molecular markers associated with cancerous growth. This targeted approach minimizes the risk of false positives and enhances the reliability of the diagnostic process. As a result, individuals undergoing the PCA3 test can benefit from a more accurate assessment of their prostate health.
While the PCA3 test provides valuable insights, a definite diagnosis of prostate cancer is typically confirmed through a biopsy. This involves the collection of tissue samples from the prostate gland for microscopic examination. The combination of PCA3 testing and biopsy allows healthcare professionals to comprehensively evaluate the presence and nature of cancerous cells, enabling a more informed treatment decision.
As the medical field continues to advance, the integration of innovative technologies and diagnostic tools like the PCA3 test holds the potential to revolutionize prostate cancer detection and management. Individuals can now benefit from enhanced accuracy, early intervention, and improved outcomes in their journey towards optimal prostate health. Note: This blog was written in 2023 and this is the information given to me as I was researching.
.
 ..
..
10. HOW FAST DOES PROSTATE CANCER GROW?
Determining the aggressiveness of prostate cancer presents a significant challenge, as treatment decisions hinge on balancing potential side effects like incontinence and impotence against the need to manage the disease effectively. It’s important to note that many prostate cancers tend to be slow-growing in nature. Remarkably, post-mortem examinations have revealed a surprising statistic: around 80 percent of men aged 80 or older possess cancer cells within their prostates that may have existed for 20 to 25 years, yet these cells often don’t contribute to their cause of death.
This intricate balance underscores the complexity of prostate cancer management. The medical community faces the task of discerning between cases that require immediate intervention and those where watchful waiting or less aggressive treatments might be more appropriate. Striking the right balance is vital to optimizing both the patient’s quality of life and their long-term well-being.
Recent advancements in medical technology and research have aimed to refine the ability to differentiate between aggressive and slow-growing prostate cancers. These advancements empower healthcare professionals to make more informed decisions tailored to each patient’s unique circumstances. As we continue to delve into the intricacies of prostate cancer behavior, ongoing research seeks to enhance our understanding and refine treatment approaches for better patient outcomes.
.
Thirteen Facts Prostate Health
11. KEY FACTORS FOR PROSTATE CANCER TREATMENT
Medical practitioners determine the appropriate course of treatment by carefully considering several key factors, including the individual’s age, the perceived aggressiveness of the cancer, results from the prostate-specific antigen (PSA) test, and the patient’s own attitude towards treatment options. This comprehensive assessment allows doctors to tailor their approach to each patient’s unique circumstances, maximizing the chances of successful outcomes and preserving quality of life.
Among every 100 men diagnosed with prostate cancer, approximately two-thirds undergo aggressive treatment methods. These treatments may involve surgical procedures, radiation therapy, or other interventions aimed at directly targeting and eradicating the cancer cells. The decision for aggressive treatment is typically made when the cancer is deemed to pose a significant threat and necessitates immediate action.
Conversely, the remaining one-third of patients choose a more cautious approach, opting for active surveillance and monitoring. This strategy involves regular follow-up appointments, which include blood tests, biopsies, and digital rectal examinations.
By carefully monitoring the cancer’s progression over time, healthcare professionals can intervene if the cancer shows signs of becoming more aggressive. This approach is particularly suitable for cases where the cancer is slow-growing or less likely to cause immediate harm.
The ultimate goal of these tailored treatment decisions is to achieve the best possible outcomes for patients while minimizing unnecessary side effects. By considering the individual’s age, cancer characteristics, and personal preferences, medical practitioners strive to strike a delicate balance between effective treatment and maintaining the patient’s overall well-being.
.
Thirteen Facts Prostate Health
12. THE SIDE EFFECTS OF PROSTATE CANCER TREATMENT
Prostate cancer treatment options, such as surgical removal of the prostate, radiotherapy, as well as innovative techniques like freezing (cryotherapy) or heat treatment (high-intensity focused ultrasound, or HIFU), have evolved significantly in recent years. These advancements have contributed to reducing the occurrence of serious side effects that were once associated with these treatments.
Importantly, many individuals undergoing prostate cancer treatment experience minimal to no side effects. Surgical procedures, such as prostatectomy, have become more refined, allowing for better preservation of surrounding tissues and nerves, thus minimizing the risk of complications like incontinence and erectile dysfunction. Radiotherapy techniques have also become more targeted, reducing damage to healthy tissue and limiting adverse effects.
Cryotherapy and HIFU, relatively newer approaches, are designed to selectively target and destroy cancerous tissue while minimizing harm to nearby structures. These methods harness precise temperature changes to eradicate cancer cells, which can lead to fewer side effects compared to traditional treatments.
While each treatment option has its own set of potential side effects, advancements in medical technology and techniques have significantly mitigated their severity. For instance, urinary and sexual function preservation has improved due to refined surgical methods, and radiotherapy advancements have reduced bowel and urinary complications.
Moreover, the availability of comprehensive supportive care strategies, including physical therapy, dietary guidance, and counseling, further helps manage and alleviate any potential side effects that may arise from treatment. It’s essential for patients to have open and informed discussions with their healthcare providers about potential side effects, treatment options, and the best approach for their individual case.
This collaborative decision-making process empowers patients to choose a treatment plan that aligns with their medical needs and personal preferences, while striving for the optimal balance between effective cancer control and maintaining their overall quality of life.
.

.
13. LYCOPENE AN ANTIOXIDANT IS GOOD FOR THE PROSTATE
The positive impact of tomatoes on prostate health has been extensively supported by various scientific investigations. Lycopene, a potent antioxidant and natural pigment found abundantly in tomatoes, has shown promising associations with lowering the risk of prostate cancer.
Numerous research studies have consistently revealed that individuals who include lycopene-rich foods in their diet, particularly tomatoes and tomato-based products like tomato sauce, tomato paste, and even watermelon, exhibit a decreased susceptibility to developing prostate cancer. Lycopene’s antioxidant properties play a crucial role in neutralizing harmful free radicals in the body, which are linked to cancer development.
Furthermore, engaging in regular physical activity has emerged as another valuable aspect of maintaining prostate health. Physical exercise has been linked to a range of health benefits, including better hormone regulation, enhanced immune function, and improved circulation, all of which contribute to a reduced risk of prostate cancer.
Adopting a well-rounded diet that features a variety of fruits and vegetables beyond just tomatoes can further bolster prostate health. Consuming a diverse array of colorful produce provides essential vitamins, minerals, and antioxidants that collectively support overall well-being and may have a protective effect against prostate cancer.
In addition to dietary choices and exercise, maintaining a healthy weight is crucial. Excess body weight, particularly abdominal fat, has been associated with an increased risk of prostate cancer and other chronic diseases. Achieving and maintaining a healthy weight through balanced nutrition and regular physical activity is integral to promoting prostate health.
Lastly, avoiding smoking is essential for both overall health and prostate well-being. Smoking is a well-known risk factor for numerous cancers, including prostate cancer. Quitting smoking can significantly contribute to reducing the risk of various health complications, including prostate cancer.
Incorporating these habits into a proactive lifestyle can significantly contribute to supporting and maintaining prostate health. It’s important to consult with a healthcare professional before making any significant changes to your diet or exercise routine, especially if you have existing health conditions or concerns.
.
Thirteen Facts Prostate Health
THE MALE PROSTATE GLAND — Problems that he may experience as he ages…
.
SCAR TISSUE FROM PROSTATE BRACHYTHERAPY CANCER TREATMENT — A 52 Year Old Male’s Story
.
.
.
MY BLOG
I do hope that you enjoyed reading my blog about the 13 critical aspects of male prostate health both informative and valuable. If you have any further questions or would like to explore this topic in more depth, please don’t hesitate to reach out. Your commitment to raising awareness about male prostate health is commendable, and I’m here to support your efforts in promoting overall well-being and health education.
.
.
.
Thirteen Facts Prostate Health
 Written on August 9th, 2013 by Aleena Aspley, who is a Certified Sexological Bodyworker.
Written on August 9th, 2013 by Aleena Aspley, who is a Certified Sexological Bodyworker.
Aleena is open to seeing people of all genders and sexual orientations. Her Somatic Sexology & Intimacy Coaching NEO Tantric bodywork studio is located in North Brisbane, Queensland Australia.
.
.
MY WEBSITES
Women: YoniWhisperer.com.au
Couples: TantricWhisperer.com
My Bodywork Directory – AleenaAspley.com/
.
.
.
.
MY CONTACT DETAILS
Ms. Aleena Aspley
Certified Sexological Bodyworker / Somatic Sex Educator
NEO Tantra & Chakrassage Professional
.
.
My Bodywork Studio: North Brisbane, Queensland
Phone: 0404 449 433 (Text me to Book)
Overseas: +61 404 449 433
By Appointment: Monday to Friday until 9pm
I work occassional weekends – just ask
My Bodywork Directory – www.AleenaAspley.com
Thirteen Facts Prostate Health
.
.
.
Thirteen Facts Prostate Health
